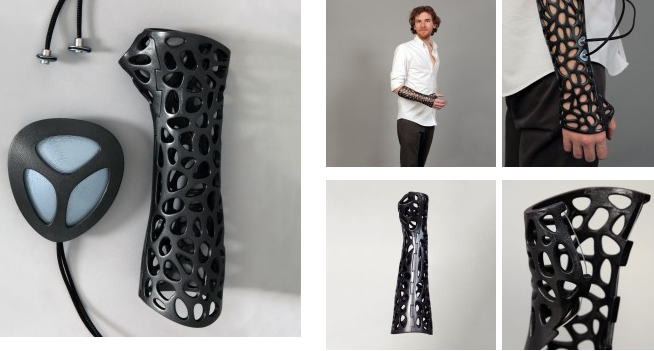
Osteoid Medical cast, attachable bone stimulator by Deniz Karasahin won a design award.
In order to function, the LIPUS ultrasound probes has to be placed on the injured area with direct skin contact, because of this requirement it was not possible to use this method with patients using standard medical casts. Now thanks to the ventilation holes on the Osteoid medical cast the LIPUS bone stimulator probes can be placed over the injured area. The LIPUS probes are attachable to the Osteoid medical cast. There is a thin layer of rubber fixed to the edges of the LIPUS adapters, this rubber layer helps these pieces to fit on the ventilation holes of the medical cast.
How does ultrasound benefit wound healing?
Inflammatory Phase – ultrasound causes a degranulation of mast cells resulting in the release of histamine. Histamine and other chemical mediators released from the mast cell are felt to play a role in attracting neutrophils and monocytes to the injured site. These and other events appear to accelerate the acute inflammatory phase and promote healing.
Proliferative Phase – ultrasound has been noted to effect fibroblasts and stimulate them to secrete collagen 1. This can accelerate the process of wound contraction and increase tensile strength of the healing tissue 2. Connective tissue will elongate better if both heat and stretch are combined. Continuous ultrasound at higher therapeutic intensities provides and effective means of heating deeper tissue prior to stretch.
RESEARCH ABSTRACT:
The LIPUS pulse generator and the nature of healing with LIPUS was the primary focus of their literature review
Abstract
Sixty-seven closed or grade-I open fractures of the tibial shaft were examined in a prospective, randomized, double-blind evaluation of use of a new ultrasound stimulating device as an adjunct to conventional treatment with a cast. Thirty-three fractures were treated with the active device and thirty-four, with a placebo control device. At the end of the treatment, there was a statistically significant decrease in the time to clinical healing (86 +/- 5.8 days in the active-treatment group compared with 114 +/- 10.4 days in the control group) (p = 0.01) and also a significant decrease in the time to over-all (clinical and radiographic) healing (96 +/- 4.9 days in the active-treatment group compared with 154 +/- 13.7 days in the control group) (p = 0.0001). The patients’ compliance with the use of the device was excellent, and there were no serious complications related to its use. This study confirms earlier animal and clinical studies that demonstrated the efficacy of low-intensity ultrasound stimulation in the acceleration of the normal fracture-repair process
Low-Intensity Pulsed Ultrasound and Pulsed Electromagnetic Field in the Treatment of Tibial Fractures: A Systematic Review (2007) compare the effects of low-intensity pulsed ultrasound (LIPUS) or pulsed electromagnetic fields (PEMF) on fracture healing through a systematic review of original, English-language clinical research reports.
Current methods of fracture care use various adjuncts aimed at decreasing time to fracture union and improving fracture union rates. Among the most commonly used modalities, low-intensity pulsed ultrasound is emerging as a safe, cost-effective and reliable treatment for both fresh fractures and fracture nonunions. Both in vivo and in vitro basic science studies have helped to elucidate potential mechanisms of ultrasound action and a number of prospective, randomised, double-blind, placebo-controlled trials exist demonstrating the clinical efficacy of low-intensity pulsed ultrasound. This article will review the evidence for the use of low-intensity pulsed ultrasound in fracture care.
Prior works: Jake Evill: Cortex, http://www.evilldesign.com/cortex Nicholas Solakian, Peter Nguyen, and Derek Buell: Splint, http://www.popsci.com/technology/article/2013-08/intricate-3-d-printed-exoskeleton-splints#comments Julian Grote: 3D printed Cast, http://www.juliangrote.com/59817/2013031/work/3d-printed-cast
If you liked this article, please give it a quick review on ycombinator or StumbleUpon. Thanks

Brian Wang is a Futurist Thought Leader and a popular Science blogger with 1 million readers per month. His blog Nextbigfuture.com is ranked #1 Science News Blog. It covers many disruptive technology and trends including Space, Robotics, Artificial Intelligence, Medicine, Anti-aging Biotechnology, and Nanotechnology.
Known for identifying cutting edge technologies, he is currently a Co-Founder of a startup and fundraiser for high potential early-stage companies. He is the Head of Research for Allocations for deep technology investments and an Angel Investor at Space Angels.
A frequent speaker at corporations, he has been a TEDx speaker, a Singularity University speaker and guest at numerous interviews for radio and podcasts. He is open to public speaking and advising engagements.