There is a large scale study using 1000 mice testing four major life extension therapies to see if there is an additive effect and how much additive effect there is. Preliminary data is show there can be longer lifespans with combined therapies.
There have been different life extension therapies where each on there own can add about 10-35% to the remaining life of a mouse. Here we are seeing if combining four of the best therapies can more than double the expected remaining life of a middle age mouse from one year to over two years.
Those four interventions are:
* Senescent cell ablation via galactose-conjugated Navitoclax (“Nav-Gal”)
* Rapamycin in food at 42 ppm
* Enhanced telomerase expression via repeated TERT gene therapy (via nasally administered AAV-mTERT)
* Hematopoietic stem cell transplantation
mTERT is telomerase. This is preventing or reducing the erosion of the end pieces of DNA. Telomerase is an enzyme that can lengthen telomeres, which are caps on the ends of chromosomes that protect DNA from damage. Telomerase can prevent some cells, like stem cells, from declining and dying as they divide. Telomere length can be measured from blood DNA using the polymerase chain reaction (PCR) test. Telomere length shortens by about 30–35 base pairs (bp) per year, on average. According to a study, people with shorter telomeres have higher mortality rates from heart and infectious diseases. However, evidence suggests that telomeres alone don’t determine lifespan.
The macrolide drug rapamycin inhibits TORC1 activity and can extend lifespan in model organisms, including mice. In mice, rapamycin can delay several age-related diseases, such as cognitive decline, spontaneous tumor and cardiovascular and immune dysfunction.
Aubrey de Grey describes the emerging story. The experiment has not reached the stage where conclusions can be made. However, there are clear indications of trends and preliminary expected conclusions.
Observations and My Expectations IF Trends Hold
ALERT – This section has my observations and speculation on preliminary data. The researchers must complete their experiments and work and provide their conclusions analysis.
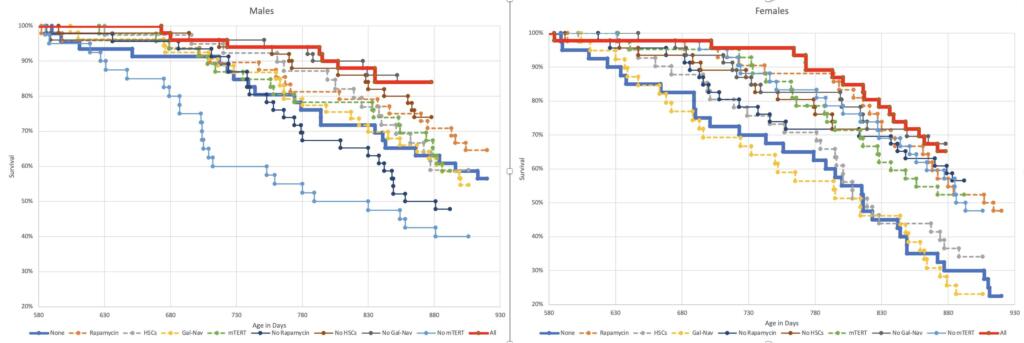
When I, Brian Wang- Nextbigfuture, observe the survival curves, it appears that the no treatment male mice are heading to about the 945 days for 50% life expectancy. It should also likely track to 1200-1300 days for 10% survival maximum life expectancy. The male mice all four treatments survival curve is about 120-200 days beyond the no treatment survival. This would mean 1065-1145 days for all-treatment reaching 50% survival. Everything started at 580 days. This means 365 days from start to 50% for no treatment and 485 to 565 days for all treatment for remaining life. This would be 33-56% improvement range for remaining life.
Rapamycin alone is about 50-days better than no treatment in male mice. All four treatment is about 100-150 days better than Rapamycin alone in male mice.
Rapamycin alone is about 80-150-days better than no treatment in female mice. All four treatment is about 20-60 days better than Rapamycin alone in female mice. The rapamycin only for females had 915 days for 50% life expectancy. The no-treatment females had about 815 days for 50% life expectancy. It looks like the all four treatment for females will have 140 days better than no-treatment. This would be 955 days. This is 235 days to 50% survival for no treatment remaining life. This is 375 days for all treatment. This is 59% better on remaining life for all four treatments.
The time to go from 85% survival to 50% survival seems to be about 250 days.
So far, once the decline in survival gets pronounced where it drops below 80-90% then the pace of decline in survival tracks roughly the same.
The female mice seem to be tracking to the no treatment group hitting 10% survival at 970 days. The all-treatment females appear to be tracking to 1100-1150 days for 10% survival. This would be 390 days remained for the notreatment group and 520-570 for the all treatment group.
Aubrey de Grey Provided His Preliminary Review Thus Far
There’s a bit of a story emerging, however, concerning the relative benefit of the interventions. I think we’re starting to be able to say that rapamycin and mTERT are more beneficial, in both sexes, both individually and in combination, than HSCs and Gal-Nav. In males the anomalously poor-performing three-intervention groups are those that lack rapa and mTERT, and rapa-only is the best single intervention. In females, similarly, Gal-Nav and HSCs are the single-intervention groups that are performing the worst, not really distinguishable from all-controls, and reciprocally the no-HSC and no-Gal-Nav groups are doing about as well as the all-four group while the other two three-intervention groups are doing slightly worse. It’s far too early to describe this as anything more than a hint of a trend, but I’ll be watching it to see if it persists.
The HSC and Gal-Nav treatments are underperforming, that could be because they are just not benefiting the mice, or it could be that the benefits are being counteracted by negative effects of the delivery process. The latter is quite plausible because multiple injections were required.

And you’ll immediately see that the stories for HSCs and for NavGal are significantly different. In the case of HSCs, as of now it looks rather strongly as though the delivery process explains most of the poor performance in males, but little or none of the poor performance of females. In the case of GalNav, on the other hand, delivery doesn’t seem to explain much. But another quite conspicuous aspect of these curves is how they compare early on. For both HSCs and GalNav, for quite a long time (up to age 800 days or so), the MOCK females did quite considerably better than the NAIVE ones! I’m definitely at a loss to explain that.
The biggest questions are still a few months away from being answered, though. I’m talking, of course, about the impact on maximum lifespan (which, as is conventional, we will define as the point when only 10% of the cohort is alive).
Fine Tuning Combination and Improving Delivery
IF the stem cells and senolytics had delivery and other problems, then fixing those issues and fine tuning the combination therapy could result in an improvement of another 100 days in life for the mice.
I expect that three to ten more attempts with different combinations with fine-tuned treatments and delivery look like doubling remaining life is possible. This could move up from 40-60%.
Another aspect that should be tested is to perform monitoring and measurements of blood and other physiology to see if there would be gains from adjusting the protocols and treatments for individuals. DNA and autopsy screening could identify mice that were less responsive to different treatments. Combining combination treatments with testing of patients before and during treatment.
We still need to see the full remaining year of results for this experiment and the autopsy and other analysis of these mice.

Brian Wang is a Futurist Thought Leader and a popular Science blogger with 1 million readers per month. His blog Nextbigfuture.com is ranked #1 Science News Blog. It covers many disruptive technology and trends including Space, Robotics, Artificial Intelligence, Medicine, Anti-aging Biotechnology, and Nanotechnology.
Known for identifying cutting edge technologies, he is currently a Co-Founder of a startup and fundraiser for high potential early-stage companies. He is the Head of Research for Allocations for deep technology investments and an Angel Investor at Space Angels.
A frequent speaker at corporations, he has been a TEDx speaker, a Singularity University speaker and guest at numerous interviews for radio and podcasts. He is open to public speaking and advising engagements.


Mice are notoriously short-lived, which is why they are used for fast results in experiments. But in longevity experiments, mice may be the least useful mammal. The dog experiments will tell us more, but only long term human trials will be decisive, and people alive an old today can’t wait that long so they’ll want to try these things on their own.
Another note on mice from my personal experience as a lab technician responsible for caring for 100-150 mice (the higher number at the end of my 8-month high school stint). Mice are also notoriously hard to feed precisely. Their appetites differ by species/subspecies, individually, and with respect to food given. Even if you measure food precisely, and even if the mice have no cage mates (which is detrimental in other ways), there’s no guarantee they will eat it all. Exercise is a factor too, and this too differs in all these ways.
Diet then, is a factor in these experiments even if unintended. It will undoubtedly matter as much or more in long-lived humans, perhaps over-whelming the effects to the 4-model treatments.
I’m curious why they didn’t use simple agents like Nrf2 inducers (e.g., benfotiamine and sulforaphane), which boost Klotho expression in places like the heart and kidneys (also good for hippocampal aging). I’ve seen high doses stabilize and slightly reverse heart and kidney failure in an elderly patient whom a doctor only gave a few more months to live. (Good evidence these also protect against ALS/FTD.)
The gut flora product butyrate is also a proven life-extension agent. The SCFA is produced by friendly flora digesting prebiotic fiber like inulin (FOS). Butyrate elevates GLP-1 (and laughably cheap compared to Ozempic). Its epigenetic actions (HDAC inhibition) partly overlap with AMPK activator metformin (which itself overlaps with mTOR inhibition). Unique among HDAC inhibitors, butyrate doesn’t elevate RAGE/TLR4 ligand HMGB1 and butyrate deficiency is associated with neurodegenerative disorders like ALS, Alzheimer’s and Parkinson’s (which I personally theorized about and started tracking nearly a dozen years ago).
Studies also point to the importance of gut health in aging – but not just proper bacterial populations; helminths (worms) are also crucial. The CHOP domains shed by helminths to manipulate the host ought to limit the IL-1beta/IL-6 pathways overactivated in aging, but also in chronic inflammatory disorders like multiple sclerosis, arthritis, atherosclerosis and endometriosis. Western society suffers from an excess sympathetic/parasympathetic balance – or, in other words, a deficiency in vagal tone. Deworming has been a major contributor to this. (There’s increasingly good evidence that deworming has left us vulnerable to RNA respiratory viruses (big driver in autism and schizophrenia), though their immune-shifting can be debilitating for other infections like TB. Also, there’s some interesting cross-talk between helminth colonizations and cathelicidins (which also come off vitamin D3/VDR, butyrate and HIF-1alpha pathways). Cathelicidin has been linked to preventing Alzheimer’s (which I predicted back in 2010) and Parkinson’s (which surprised me this week when I found it on a deep dive in Pubmed.))
Cholinergics turn out to be quite important for stem cells niche maintenance. Unfortunately, for many people there may be no easy way to simply supplement choline to compensate for this cholinergic deficiency (e.g., TMAO). There’s some indication citicoline may work – and there’s the p75NGFR activator/AChE inhibitor acetylcarnitine, but that’s problematic. Some have suggested uridine and DHA to boost choline synthesis – but this may never be an equivalent that compensates for the loss of these commensal organisms that have been manipulating our immune systems throughout our evolution.
DHA brings me to essential fatty acids. GLA is a cheap life extension agent as well, though it too has potential drawbacks. ALA inhibits soluble epoxide hydrolase, which gives you oxylipins and good blood pressure (but watch the phosphate load in flax seeds). Western diets are deficient in both ALA and GLA. Instead we’re shifted towards AA and palm oil (TLR4)/fatty acid synthase – crucial to viral propagation and cancer. We’ve known a long time that TLR4/sympathetic overactivation drives heart failure (cardiomyopathy), but good luck getting your cardiologist to think diet can save your cardiovascular system (“Ain’t no reimbursement kickback on that! What are ya doin’? Yer cuttin’ into my executive bonus money! Gotta have that bonus money, baby!”)
If you’re already using HPSCs, why not boost MIRO-1 to enhance mitochondrial transfer? There’s evidence hypoxic pretreatment or sulfhydration of HPSCs could also boost effectiveness (LL-37 again?). There are also ways to restore depressed H2S production besides AMPK, like – for instance – a little molybdenum and B6. Boron also pops up on the radar. Certain trace minerals are often overlooked.
Finally, folates (or methyl-B12) can’t be used orally without a backfire effect, but they can be injected. This has been overlooked in favor of methionine restriction (been there, done that and it’s no fun).
I’m sure some of these life extension approaches would overlap, but some of them are quite cheap and have few drawbacks.
Agree 100% on the diet issue. Doctors know little to nothing about diet influences & contradict each other and the also ignorant & compromised USDA recommendations.
My cholesterol has been high my whole life, even on meds. Without meds, like now, it can tip over 300mg total.
I finally asked my doctor “well, can we run a test to see if I actually have artery blockage?” I suspected I did not because I have been getting regular ultra-sound tests from an outside medical service that specializes in that, but my doctors all dismissed that test and didn’t run it themselves.
My doctor prescribed a Calcium CT test. It came back with zero percent blockage, a perfect score. He told me to just keep on doing what I’ve been doing for most of my 65 years on Earth.
I believe it’s the sugar, or lack of, in my foods, plus heart-pounding exercise, that’s responsible for my results. My father had a different diet and needed a double bypass about 10 years before the age I am now.
I cut out almost all foods with added sugar: no sodas, cake, cookies (fresh fruit instead for “sweet things”), minimal low sugar cereals (2-3 small boxes/year), very little processed food of any kind. Mostly paleo, semi-keto but more fruits & vegies than the carnivore versions. I do eat a lot of meat at dinner though, and 4 eggs in the morning, yolk and all, despite the cholesterol hit. Egg yolks are the healthiest part of the egg, and without that there’s not much point in eating eggs.
“Studies also point to the importance of gut health in aging”
I’ve personally wondered about the impact of antibiotics on gut biome and aging.
A substantial portion of human breast milk, (Which is very different from cow milk!) consists of complex sugars, “human milk oligosaccharides”, not intended to be digested by the baby, but instead by gut bacteria. It’s a way of encouraging acquisition of a proper gut biome.
Later in life we go through all sorts of events that might screw up said biome. I wonder if regular consumption of HMOs might slow some of the symptoms of aging?
The FOS I mentioned is fructo-oligosaccharides, which are digested by healthy flora to produce butyrate and other SCFA. Butyrate retards Parkinson’s and Alzheimer’s, so the answer to your question appears to be yes. The sugars in human milk are particularly tailored for human flora so that they’ll take root but other components are important too like tryptophan derivatives.
“I expect that three to ten more attempts with different combinations with fine-tuned treatments and delivery look like doubling remaining life is possible.”
Do you realize it takes 2 to 3 years just to do one attempt ? I don’t think doing this for decades is viable. Doing it just one or two times just to prove RMR is ok. Ideally we would like to test it on millions virtual humans, but insillico trials are still at least 10 years away.